Mental Health and COVID-19: The Psychological Implications of a Pandemic for Nurses
Background: The risk of psychological effects from the COVID-19 pandemic is significant and manifests as stress, anxiety, depression, sleeplessness, and, in some cases, suicide. The need for psychological support services for healthcare providers should be included in all pandemic and disaster planning.
Objectives: The aim of this article is to explore the potential psychological sequelae of nursing during a pandemic and to provide recommendations to support a psychologically healthy work environment.
Methods: Highlights from the literature on psychological sequelae, symptoms, and outcomes related to COVID-19 and prior pandemics is presented, along with insight from the experiences of oncology nurses caring for patients with COVID-19.
Findings: Destigmatizing mental health needs for healthcare providers empowers them to seek support. Hospital administrators must develop proactive wellness plans for the triage and management of mental and emotional health needs during a pandemic that prioritize transparent communication, resources for healthcare providers within and beyond the clinical setting, and training.
Jump to a section
Since the first COVID-19 cases were reported in December 2019, more than 37 million individuals have been diagnosed worldwide, including nearly 8 million cases in the United States alone (World Health Organization, 2020). Of the more than 1.9 million deaths to date, more than 400,000 have occurred in the United States; more than 1,500 have been healthcare workers (Reed, 2020; World Health Organization, 2021). The psychological burden of the pandemic from both a personal and professional perspective has contributed to stress, anxiety, depression, and, in some cases, suicide among healthcare professionals (Mahbubani & Mosher, 2020). The endemic nature of the pandemic has required increased attention to how best to support healthcare providers, including nurses, as they cope with the stresses of the pandemic at work and home. The causes of psychological impact for healthcare professionals include the sheer volume of individuals affected, the risk of infection, the potential rationing of care, possible shortages of personal protective equipment (PPE), the challenge of balancing work and personals demands, and the deaths of patients and coworkers (Shanafelt et al., 2020). The presence of COVID-19 symptoms may further exacerbate psychological effects, up to and including post-traumatic stress (Chew et al., 2020; Spoorthy et al., 2020).
In the context of oncology care, these risks and stressors are further magnified for patients and providers. From the outset of the pandemic, individuals with cancer were identified among those at highest risk for significant complications of COVID-19 (Robilotti et al., 2020). In addition to the potential physical sequelae, a number of psychological effects are also a concern for individuals with cancer. These effects include increased fear of contracting COVID-19; treatment delays; experiencing a new diagnosis or initiation, continuation, or completion of treatment alone; and potentially end of life and death accompanied by few, if any, family members (Young et al., 2020). Among individuals with cancer, one study demonstrated that risk of mental health complications was associated with a history of a mental health diagnosis, frequency of worrying about cancer management during the COVID-19 pandemic, higher levels of pain and fatigue, excessive alcohol consumption, and more frequent experience of psychological pressure related to COVID-19 (Wang et al., 2020). This psychological pressure manifests not only for patients with cancer, but also for the healthcare providers entrusted with their care. These individuals, most notably nurses, may assume the psychological stressor of caring for a vulnerable population who would be at risk for significant morbidity and mortality if they contracted the virus, as well as face potential barriers to providing the full scope of care to which they are accustomed (Tichich, 2020). Coupled with the additional stressors of COVID-19 at work and in the community, this creates a context for psychological sequelae for oncology healthcare professionals.
Background
Experiences from previous natural disasters provide key insights into how the stress of healthcare crises can affect the psychological well-being of providers (Krystal & McNeil, 2020). Previous pandemics, such as severe acute respiratory syndrome (SARS) and influenza A virus subtype H1N1 (H1N1), have led to negative mental health consequences for healthcare providers, including nurses (Blake et al., 2020). However, unlike weather and even previous disease-related crises that have been largely regionally confined, COVID-19 has affected health care at a global scale and created unique stressors and challenges, particularly for nurses on the front line of care (Maben & Bridges, 2020). These stressors and challenges include moral and ethical distress related to the reality that not everyone can be treated and that limited resources must be allocated (Maben & Bridges, 2020). These logistical and psychological challenges may manifest in unique ways for oncology nurses, who are caring for vulnerable, often immunocompromised patients who may be at greater risk for complications or death (Paterson et al., 2020). In addition, while nurses cope with the challenges of the pandemic in the workplace, they simultaneously do so as members of society, where they may face similar challenges related to child care, access to needed resources, and uncertainty and concern for infection inside and outside the clinical setting.
The aim of this article is to review literature about psychological effects, symptoms, and outcomes for healthcare professionals during a pandemic.
Methods
As an example of the psychological effects of the COVID-19 pandemic, this article presents stressful psychological experiences relayed by oncology nurses in acute care practice at Northwell Health Huntington Hospital in New York. In addition, to inform strategic planning during future pandemics and other natural disasters, this article reviews actions to support the well-being of healthcare professionals.
Findings
Historical Context
COVID-19 is not the first pandemic in the modern era to challenge healthcare providers. The H1N1 pandemic led to 60.8 million cases, 274,304 hospitalizations, and 12,469 deaths in the United States from April 2009 to April 2010 (Centers for Disease Control and Prevention, 2019). In addition, although SARS and the Middle East respiratory syndrome (MERS) had high mortality rates (10%), they had lower transmission rates (Virginia Commonwealth University Health, 2020). A history of pandemics and the psychological influence of and sequelae from their occurrence suggest that not only do pandemics affect the psychology of individuals and communities, but their spread, duration, and intensity are also influenced by the psychological response of communities to the pandemic itself (Taylor, 2019). The context of ever-evolving healthcare delivery and demands on clinicians and health systems, coupled with the unpredictability of pandemic emergence, require creative solutions to prepare for global health challenges and particularly the mental health needs of clinicians in diverse geographic and practice settings.
Psychological Outcomes of a Pandemic for Healthcare Professionals
Although the evidence related to COVID-19 specifically is still emerging and the psychological effects may not be fully appreciated for many years to come, preliminary studies and systematic reviews provide insight into the mental health consequences of the pandemic for healthcare professionals. A systematic review and meta-analysis of articles related to COVID-19 identified poor sleep quality, stress, psychological distress, insomnia, post-traumatic stress, anxiety, and depression secondary to COVID-19 (Krishnamoorthy et al., 2020). In that review, healthcare workers had one of the highest psychological symptom burdens, second only to individuals who were positive for COVID-19 (Krishnamoorthy et al., 2020). A second meta-analysis reported a pooled prevalence of anxiety (23%), depression (28%), and insomnia (39%) among healthcare professionals, with female healthcare providers and nurses demonstrating higher rates of affective symptoms (Pappa et al., 2020). A broader review examined mental health outcomes of healthcare professionals (n = 60,458) exposed to SARS, MERS, or COVID-19 (de Pablo et al., 2020). Symptoms observed across 115 publications included fear (44%), insomnia (38%), psychologic distress (38%), burnout (34%), anxiety (29%), depressive symptoms (26%), post-traumatic stress disorder (PTSD) (21%), somatization (16%), and stigmatization (14%) (de Pablo et al., 2020). In a study of nurses working in hospitals treating patients with COVID-19, 25% were identified as experiencing psychological distress (Nie et al., 2020). According to the Anxiety and Depression Association of America (ADAA, 2020), stress and anxiety can evolve into acute stress disorder, which precedes PTSD, of which the latter is chronic. Depressive symptoms are likely to follow chronic unresolved anxiety. Anxiety and depressive symptoms may include constant fear, excessive worrying, poor concentration, disturbances in sleep or appetite, low energy or fatigue, and decreased motivation (ADAA, 2020).
Contributors to Psychological Distress in a Pandemic
A systematic review of qualitative studies (n = 13) focused on the experiences of nurses in the context of pandemics, including SARS, MERS, COVID-19, and avian influenza (Fernandez et al., 2020). Contributing factors identified in this review and another publication specific to COVID-19 are summarized in Figure 1. These contributing factors include fears about contracting or spreading the virus to patients, family, and coworkers. During the COVID-19 pandemic in particular, the stressors of exposure in the workplace may be compounded by the social restrictions present in the community, where social distancing and stay-at-home recommendations have been associated with increased depression, acute stress, and generalized anxiety disorder (Marroquín et al., 2020). The social isolation coupled with self-imposed isolation practiced by some nurses, such as staying at a hotel or away from home so as not to put family members at risk for infection, could further compound the psychological effects of a pandemic scenario. 
Beyond Psychological Outcomes
The outcomes of a pandemic transcend the psychological symptoms noted previously and can have far-reaching and potentially dire consequences, including suicide (Gunnell et al., 2020; Sher, 2020). Reports of healthcare professionals’ suicides during the COVID-19 pandemic (Dean, 2020) are a significant consequence of the mental health effects of COVID-19 that requires proactive attention to the mental health and well-being of healthcare providers. Global studies suggest that increased fear of COVID-19 is associated with psychological distress, job dissatisfaction, and increased turnover at the organizational and professional level (Irshad et al., 2020; Labrague & de los Santos, 2020). Such outcomes are consistent with studies outside the context of a pandemic that suggest that workplace stressors are a major contributor to nurse turnover (Halter et al., 2017) and reduced retention, including among oncology nurses (Gillet et al., 2018; Wu et al., 2016).
Oncology Nurse Narratives From New York
Northwell Health Huntington Hospital is a full-service, 306-bed, four-time Magnet®-designated community hospital in New York, which was the epicenter of the early COVID-19 outbreak in the United States. The Northwell Health Cancer Institute is home to the Don Monti Cancer Center, a 20-bed inpatient unit, and a five-chair outpatient infusion center. At Northwell Health Huntington Hospital, the first patient who was positive for COVID-19 presented on March 10, 2020, after which positive cases began to surge, many of which required intensive care. From March 10, 2020, through April 8, 2020, 26 hospital units were converted to care for all patients with COVID-19, leaving two areas to house uninfected medical-surgical patients. A total of 1,116 patients with COVID-19, including 96 individuals with a cancer diagnosis, were treated at Northwell Health Huntington Hospital. Of the 2,115 employees, as of August 17, 2020, 175 employees contracted the virus and 1 employee died. This resulted in many of the psychological effects highlighted previously.
Northwell Health Huntington Hospital experienced a large number of positive patient and provider cases, from which they also experienced deaths, some of whom died shortly after presenting with symptoms. This included an RN who died seven days after presenting to the hospital with flu-like symptoms. This was not only the loss of a respected colleague, but also the loss of any security felt from the use of PPE. The concern about contracting the virus within and beyond the healthcare setting, as well as the potential risk of exposure to family and friends, became a significant stressor. This is epitomized in the case of two nurses from this institution.
A new graduate nurse working on the oncology unit coped with her first patient death related to COVID-19 on the same day she went home to discover that her grandfather had died from COVID-19 after infection in the nursing home in which he resided. Just four days later, she received word that her grandmother had also died from COVID-19. She struggled emotionally with the burden of caring for patients who were dying, alongside the grief for her family members whose lives were lost. After a week of mourning, she started to feel anxious about her return to work as a nurse caring for patients with COVID-19. She experienced a myriad of emotions, including fear of returning to a clinical environment in which there was a risk of exposure to the virus that had taken the lives of her grandparents. Consistent with the literature, this nurse experienced the dual psychological challenges of experiencing death in the workplace concurrently with death related to COVID-19 in her family, resulting in fear and anxiety about returning back to work and potential risk of exposure.
A second nurse experienced the conversion of her oncology unit to a COVID-19 unit. This required a rapid translation of skills from practicing exclusively as an oncology nurse to practicing as a nurse for a highly infectious virus about which new information was constantly emerging, making it difficult to attain clinical proficiency. This transition was also highlighted by the physical manifestation of the viral presence in the form of extensive PPE. The reality of walking into a room to care for an infected patient created understandable concern. This was further exacerbated by thoughts of her own family and friends with chronic conditions who would be particularly susceptible to complications of COVID-19 if infected. These included her fiancé who has asthma, her best friend who has diabetes, and her mother who is a breast cancer survivor on lifelong immunosuppressive therapies. Several weeks later, when initiating aromatherapy for a patient, this nurse realized she could not smell. After testing positive for COVID-19, she quarantined in a bedroom in her parents’ home so as not to expose other family members. During the next few weeks, meals were left outside her bedroom door, and requests were made via text message. Although she ultimately recovered, she spent each day wondering when things were going to turn. This case highlights several contributing factors to psychological effects in nurses, including fear of contracting the virus and concern about spreading it to vulnerable family members. This led to significant physical isolation at home during a time of potentially intensified fear and emotional distress, epitomized in her concern that things would inevitably end badly. Although that nurse eventually recovered, the experience of contracting COVID-19 may contribute to persistent psychological effects.
Recommendations for Clinical Practice
Recommendations to health systems regarding ways to address mental health needs in the context of the COVID-19 pandemic were summarized by Shanafelt et al. (2020) (see Figure 2). 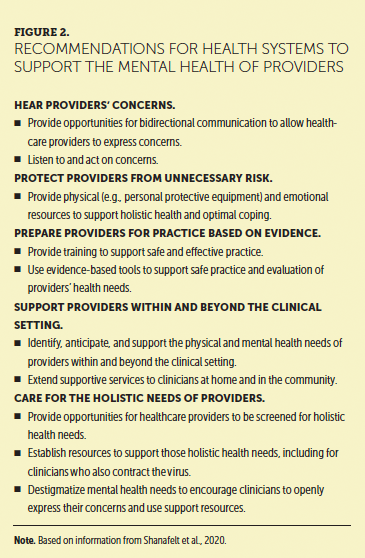
Foster an environment of psychological safety: Creating an environment of trust and support is imperative to promote a psychologically safe working environment (Rangachari & Woods, 2020). This begins with transparent communication and obtaining nurses’ insights and lived experiences to identify and address mental health needs. Focus groups can be created to discuss challenging situations that may result in mental and emotional distress for nurses. Integrating pandemic planning into new or existing educational or training programs for staff, including simulation, is imperative to provide exposure for managing patient care and self-care during a pandemic. Online forum groups can be used to aid staff and encourage opportunities to reflect and adapt to the challenges that COVID-19 may create for years to come (Veitch & Richardson, 2020).
Identify the signs of psychological distress in self and others: The ability to identify signs of psychological distress among healthcare professionals is imperative to support early intervention. In some studies, validated assessments, such as the Generalized Anxiety Disorder Scale, Primary Care PTSD Screen, or Patient Health Questionnaire–2, were used to screen for anxiety and depression (Shechter et al., 2020). Further assessment tools, including the Brief Symptom Inventory, Symptom Checklist–90–Revised, Depression Anxiety Stress Scale–21, and General Health Questionnaire–28, are validated to measure more than one domain of psychological distress (Ghawadra et al., 2019). Even without validated instruments, there are well-established signs and symptoms of anxiety, depression, and burnout in nursing (see Figure 3). They may be helpful in identifying symptom clusters indicative of one cause or more of psychological distress. These self-reported outcomes can be used by individuals to screen for the presence of psychological distress; however, such instruments should be used as part of care delivered by a healthcare professional so that any distress can be further evaluated and managed using an evidence-based approach. 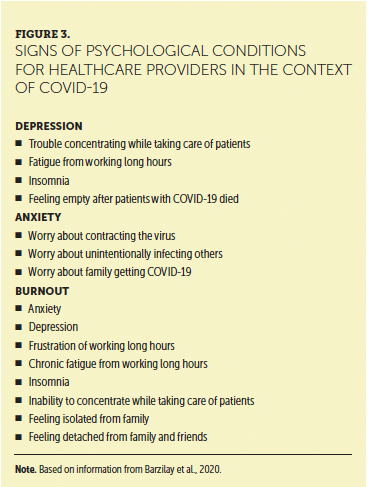
Destigmatize self-report: The stigma of mental health needs is a significant barrier to healthcare professionals self-reporting and seeking assistance (Knaak et al., 2017). Among the barriers to self-reporting is the perception of being devalued, dismissed, and dehumanized, in addition to actual or perceived discouragement from disclosing psychological challenges. The fear of being perceived as less competent or as performing work in a less reliable manner is an additional and significant barrier to seeking needed assistance (Knaak et al., 2017). Interventions, including the sharing of personal experiences of mental health needs by staff, training focused on destigmatization, and initiatives that provide a safe and supportive environment in which to self-disclose mental health needs, may contribute to destigmatization of mental health concerns among healthcare professionals and support earlier help seeking, which may, in turn, improve outcomes (Knaak et al., 2017).
The real-world experience at Northwell Health Huntington Hospital suggests the incalculable effect of COVID-19 on healthcare providers, including nurses. The long-term mental and physical effects of caring for individuals with COVID-19 remain unknown. However, early studies suggest a high prevalence of depression, insomnia, anxiety, and distress, with nurses on the front line at highest risk for experiencing symptoms of distress (Lai et al., 2020). Depending on the severity, these symptoms may begin to impair nurses’ professional function (Hu et al., 2020). Therefore, it is imperative that health systems continue to monitor for and address mental and emotional sequelae of COVID-19 and develop action plans in the event of future pandemics. Just as emergency planning is created to support the logistics of healthcare delivery in the context of man-made or natural disasters, so too should a mental health support plan be established for measuring, triaging, and treating the psychological and emotional effects of a global health crisis on healthcare providers. Northwell Health Huntington Hospital captured many of the recommendations for promoting a psychologically safe work environment, even in the most acute stages of the COVID-19 pandemic, through a series of interventions such as an emotional support resource center and “in this together” sessions that supported staff in openly sharing psychoemotional concerns related to COVID-19. 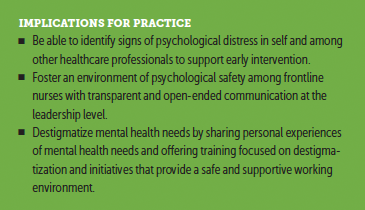
Conclusion
Few predicted a pandemic of the magnitude of COVID-19, and understanding of this pandemic, including unknown mental and emotional effects, continues to evolve. Despite this, important lessons have been learned about how to prioritize the holistic health needs of the healthcare workforce, particularly nurses. This starts by destigmatizing mental health needs for healthcare providers, empowering individuals to seek support as needed without fear of stereotype or retribution. In addition, hospital administrators must develop proactive wellness plans for the triage and management of mental and emotional health needs during a pandemic that prioritize transparent communication, resources for healthcare providers within and beyond the clinical setting, and training to ensure safe and, when available, evidence-based practice. This may be particularly important for nurses caring for specialty populations who are vulnerable to morbidity and mortality associated with COVID-19, including oncology. As evidence continues to emerge from the ongoing COVID-19 pandemic, research should focus on the longitudinal mental health outcomes for nurses and other healthcare providers, along with interventional studies to generate evidence around safe and effective approaches to prevent or ameliorate psychological distress among healthcare professionals in oncology practice and beyond.
About the Author(s)
Megha Shah, BSN, RN, OCN®, is a clinical nurse at Northwestern Medicine Cancer Center Delnor in Geneva, IL; Marie Roggenkamp, RN, BSN, MSN, OCN®, is a nurse manager, Lyndsay Ferrer, BSN, RN, OCN®, is an assistant nurse manager, and Valerie Burger, MA, MS, RN, OCN®, CPN, is the assistant vice president of cancer services, all at Northwell Health Huntington Hospital in New York; and Kelly J. Brassil, PhD, RN, FAAN, is the director of medical affairs at Pack Health in Houston, TX. The authors take full responsibility for this content and did not receive honoraria or disclose any relevant financial relationships. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Shah can be reached at theoncologynurse@gmail.com, with copy to CJONEditor@ons.org. (Submitted August 2020. Accepted October 15, 2020.)
References
Anxiety and Depression Association of America. (2020). Understand the facts: Posttraumatic stress disorder (PTSD). https://adaa.org/understanding-anxiety/posttraumatic-stress-disorder-pt…
Barzilay, R., Moore, T.M., Greenberg, D.M., DiDomenico, G.E., Brown, L.A., White, L.K., . . . Gur, R.E. (2020). Resilience, COVID-19-related stress, anxiety, and depression during the pandemic in a large population enriched for healthcare providers. Translational Psychiatry, 10, 291. https://doi.org/10.1038/s41398-020-00982-4
Blake, H., Bermingham, F., Johnson, G., & Tabner, A. (2020). Mitigating the psychological impact of COVID-19 on healthcare workers: A digital learning package. International Journal of Environmental Research and Public Health, 17(9), 2997.
Centers for Disease Control and Prevention. (2019, June 11). Influenza (flu): 2009 H1N1 pandemic. https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html
Chew, N.W.S., Lee, G.K.H., Tan, B.Y.Q., Jing, M., Goh, Y., Ngiam, N.J.H., . . . Sharma, V.K. (2020). A multinational, multicenter study on the psychological outcomes and associated physical symptoms amongst healthcare workers during the COVID-19 outbreak. Brain, Behavior, and Immunity, 88, 559–565. https://doi.org/10.1016/j.bbi.2020.04.049
de Pablo, G.S., Vaquerizo-Serrano, J., Catalan, A., Arango, C., Moreno, C., Ferre, F., . . . Fusar-Poli, P (2020). Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. Journal of Affective Disorders, 275, 48–57. https://doi.org/10.1016/j.jad.2020.06.022
Dean, W. (2020, April 30). Suicides of two health care workers hint at the Covid-19 mental health crisis to come. STAT. https://www.statnews.com/2020/04/30/suicides-two-health-care-workers-hi…
Fernandez, R., Lord, H., Halcomb, E., Moxham, L., Middleton, R., Alananzeh, I., & Ellwood, L. (2020). Implications for COVID-19: A systematic review of nurses’ experiences of working in acute care hospital settings during a respiratory pandemic. International Journal of Nursing Studies, 111, 103637. https://doi.org/10.1016/j.ijnurstu.2020.103637
Ghawadra, S.F., Abdullah, K.L., Choo, W.Y., & Phang, C.K. (2019). Psychological distress and its association with job satisfaction among nurses in a teaching hospital. Journal of Clinical Nursing, 28(21–22), 4087–4097. https://doi.org/10.1111/jocn.14993
Gillet, N., Fouquereau, E., Coillot, H., Cougot, B., Moret, L., Dupont, S., . . . Colombat, P. (2018). The effects of work factors on nurses’ job satisfaction, quality of care and turnover intentions in oncology. Journal of Advanced Nursing, 74(5), 1208–1219. https://doi.org/10.1111/jan.13524
Gunnell, D., Appleby, L., Arensman, E., Hawton, K., John, A., Kapur, N., . . . Pirkis, J. (2020). Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry, 7(6), 468–471. https://doi.org/10.1016/S2215-0366(20)30171-1
Halter, M., Boiko, O., Pelone, F., Beighton, C., Harris, R., Gale, J., . . . Drennan, V. (2017). The determinants and consequences of adult nursing staff turnover: A systematic review of systematic reviews. BMC Health Services Research, 17, 824. https://doi.org/10.1186/s12913-017-2707-0
Hu, D., Kong, Y., Li, W., Han, Q., Zhang, X., Zhu, L.X., . . . Zhu, J. (2020). Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. Journal of EClinialMedicine, 24, 100424. https://doi.org/10.1016/j.eclinm.2020.100424
Irshad, M., Khattak, S.A., Hassan, M.M., Majeed, M., & Bashir, S. (2020). How perceived threat of Covid-19 causes turnover intention among Pakistani nurses: A moderation and mediation analysis. International Journal of Mental Health Nursing. https://doi.org/10.1111/inm.12775
Knaak, S., Mantler, E., & Szeto, A. (2017). Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthcare Management Forum, 30(2), 111–116. https://doi.org/10.1177/0840470416679413
Krishnamoorthy, Y., Nagarajan, R., Saya, G.K., & Menon, V. (2020). Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Research, 293, 113382. https://doi.org/10.1016/j.psychres.2020.113382
Krystal, J.H., & McNeil, R.L. (2020). Responding to a hidden pandemic for healthcare workers: Stress. Nature Medicine, 26, 639. https://doi.org/10.1038/s41591-020-0878-4
Labrague, L.J., & de los Santos, J.A.A. (2020). Fear of Covid-19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management. https://doi.org/10.1111/jonm.13168
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., . . . Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976
Maben, J., & Bridges, J. (2020). COVID-19: Supporting nurses’ psychological and mental health. Journal of Clinical Nursing, 29(15-16), 2742–2750. https://doi.org/10.1111/jocn.15307
Mahbubani, R., & Mosher, D. (2020, April 28). Suicide is killing frontline medical workers, but mental-health experts say the situation is far from hopeless. Business Insider. https://www.businessinsider.com/coronavirus-pandemic-doctor-ambulance-w…
Marroquín, B., Vine, V., & Morgan, R. (2020). Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Research, 293, 113419. https://doi.org/10.1016/j.psychres.2020.113419
Nie, A., Su, X., Zhang, S., Guan, W., & Li, J. (2020). Psychological impact of COVID-19 outbreak on frontline nurses: A cross-sectional survey study. Journal of Clinical Nursing, 29(21–22), 4217–4226. https://doi.org/10.1111/jocn.15454
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V.G., Papoutsi, E., & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity, 88, 901–907. https://doi.org/10.1016/j.bbi.2020.05.026
Paterson, C., Gobel, B., Gosselin, T., Haylock, P.J., Papadopoulou, C., Slusser, K., . . . Pituskin, E. (2020). Oncology nursing during a pandemic: Critical reflections in the context of COVID-19. Seminars in Oncology Nursing, 36(3), 151028. https://doi.org/10.1016/j.soncn.2020.151028
Rangachari, P., & Woods, J.L. (2020). Preserving organizational resilience, patient safety, and staff retention during COVID-19 requires a holistic consideration of the psychological safety of healthcare workers. International Journal of Environmental Research and Public Health, 17(12), 4267. https://doi.org/10.3390/ijerph17124267
Reed, T. (2020, September 28). More than 1,700 U.S. healthcare workers have died from COVID-19, nurses’ union says. FierceHealthcare. https://www.fiercehealthcare.com/practices/report-how-many-u-s-healthca…
Robilotti, E.V., Babady, N.E., Mead, P.A., Rolling, T., Perez-Johnston, R., Bernardes, M., . . . Kamboj, M. (2020). Determinants of COVID-19 disease severity in patients with cancer. Nature Medicine, 26(8), 1218–1223. https://doi.org/10.1101/2020.05.04.20086322
Shanafelt, T., Ripp, J., & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA, 323(21), 2133–2134. https://doi.org/10.1001/jama.2020.5893
Shechter, A., Diaz, F., Moise, N., Anstey, D.E., Ye, S., Agarwal, S., . . . Abdalla, M. (2020). Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. General Hospital Psychiatry, 66, 1–8. https://doi.org/10.1016/j.genhosppsych.2020.06.007
Sher, L. (2020). The impact of the COVID-19 pandemic on suicide rates. QJM: An International Journal of Medicine, 113(10), 707–712. https://doi.org/10.1093/qjmed/hcaa202
Spoorthy, M.S., Pratapa, S.K., & Mahant, S. (2020). Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian Journal of Psychiatry, 51, 102119. https://doi.org/10.1001/jama.2020.5893
Taylor, S. (2019). The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Cambridge Scholars Publishing.
Tichich, E.R. (2020). Mitigating compassion fatigue and nurse burnout amid COVID-19. Oncology Nursing News. https://www.oncnursingnews.com/publications/oncology-nurse/2020/august-…
Veitch, P., & Richardson, K. (2020). Nurses need support during the COVID-19 pandemic. Journal of Psychiatric and Mental Health Nursing. https://doi.org/10.1111/jpm.12666
Virginia Commonwealth University Health. (2020, March 24). Comparing COVID-19 with H1N1 and other viral outbreaks. https://www.vcuhealth.org/news/comparing-covid-19-with-h1n1-and-other-v…
Wang, Y., Duan, Z., Ma, Z., Mao, Y., Li, X., Wilson, A., . . . Chen, R. (2020). Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Translational Psychiatry, 10, 263. https://doi.org/10.1038/s41398-020-00950-y
World Health Organization. (2020). WHO coronavirus disease (COVID-19) dashboard. Retrieved August 14, 2020, from https://covid19.who.int/?gclid=EAIaIQobChMI7siSj7fq6gIVC77ACh28KwI-EAAY…
World Health Organization. (2021). WHO coronavirus disease (COVID-19) dashboard. Retrieved January 12, 2021, from https://covid19.who.int
Wu, S., Singh-Carlson, S., Odell, A., Reynolds, G., & Su, Y. (2016). Compassion fatigue, burnout, and compassion satisfaction among oncology nurses in the United States and Canada. Oncology Nursing Forum, 43(4), E161–E169. https://doi.org/10.1188/16.ONF.E161-E169
Young, A.M., Ashbury, F.D., Schapira, L., Scotté, F., Ripamonti, C.I., & Olver, I.N. (2020). Uncertainty upon uncertainty: Supportive care for cancer and COVID-19. Supportive Care in Cancer, 28(9), 4001–4004. https://doi.org/10.1007/s00520-020-05604-9


