Nurse Attitudes: A Descriptive Study of Families’ Importance in Inpatient Nursing Care
Background: Family support and patient outcomes are linked to nurses’ attitudes toward families’ importance in patient care.
Objectives: The purpose of this study was to characterize inpatient oncology nurses’ attitudes toward families’ importance in nursing care and determine characteristics related to these attitudes.
Methods: A descriptive, cross-sectional design was used with a single set of measurements from inpatient oncology nurses at a comprehensive cancer center in the southeastern United States. Nurse characteristics were summarized using frequency and percentages. Time variables were summarized using median and interquartile range. There were five primary outcomes: Families’ Importance in Nursing Care–Nurses’ Attitudes (FINC-NA) total score and four subscale scores. Analysis of variance and Pearson correlation assessed relationships between nurse characteristics and attitudes.
Findings: Nurses considered the role of the family important, but level varied by FINC-NA item. Characteristics related to family importance overall included hospital unit and general approach to care.
Jump to a section
Patient- and family-centered care embraces four core concepts: dignity and respect, information sharing, participation, and collaboration (Institute for Patient- and Family-Centered Care, n.d.). Patients and their family members are considered vital allies of the healthcare team for quality and safety. The positions of the American College of Physicians and the Nursing Alliance for Quality Care reinforce these concepts and emphasize that patients and families should be active partners in all aspects of care (Nickel et al., 2018; Sofaer & Schumann, 2013). Growing evidence demonstrating a relationship between family support and patient outcomes suggests that this is dependent on nurses’ attitudes toward the importance of families in patient care (Luttik et al., 2017).
Background
The role of family members in the care of the patient is sometimes unclear to both nurses and the family members themselves. Nurses report the unpredictability and uncertainty of the family members’ participation as challenging (Alshahrani et al., 2018). Family members face many challenges, such as potential losses, need for information, and decision-making. Psychosocial factors that may affect a family member include mental health issues and burnout, level of understanding, family dynamics, personal views and attitudes, and language barriers (Koren et al., 2018).
A national sample of 433 critical care nurses in the United States was surveyed to determine factors that may influence family engagement (Hetland et al., 2017). Nurses were more likely to engage family members in simple daily care tasks if they were aged younger or older (compared to aged 25–49 years) and had a doctoral degree, more critical care experience, or lower staffing ratios, or worked in a rural hospital or pediatric intensive care unit (Hetland et al., 2017). Studies have also examined family members’ report of their experiences of collaboration and attitudes of staff, offering insight into areas needing improvement. In a study of relatives of older adult patients, the relatives reported evasiveness in staff attitudes and availability, a perceived absence of care, and feelings of being invisible and unrecognized (Sivertsen et al., 2018). Families report a need for communication to have their concerns considered even if the news is bad or unknown (Dahlke et al., 2018) and to be provided with postdischarge care instructions during hospitalization (Nyborg et al., 2017).
Studies using the Families’ Importance in Nursing Care–Nurses’ Attitudes (FINC-NA) instrument found differences in nurses’ attitudes toward the importance of family involvement in patient care in relation to geographic areas and demographic characteristics. Having more education and working in a research, education, or management role were significantly associated with more positive attitudes in a study comparing nurses in Scandinavia and Belgium, with the former being more positive (Luttik et al., 2017). Two additional studies with nurses in Sweden also noted overall support of families’ involvement. The first study found that being a new nurse, lacking a clearly defined institutional family approach to care, and being a male nurse predicted a less supportive attitude (Benzein, Johansson, Årestedt, & Saveman, 2008). The second study noted that there was less support for inviting families to participate in heart failure care or planning of the care (Gusdal et al., 2017). Factors predicting a more supportive attitude were working in a primary healthcare center or heart failure clinic, having received cardiac and healthcare education, and feeling competent to work with families (Gusdal et al., 2017). Attitudes of RNs and licensed practical nurses were compared pre- and postimplementation of a family systems educational program (Blöndal et al., 2014). Prior to the intervention, younger and less experienced nurses, compared to those with 7–15 years of experience, found the family more burdensome, but this was noted to improve postintervention (Blöndal et al., 2014). In addition, the investigators found that postintervention, nurses reported more positive attitudes about the family as its own resource and as a resource in nursing care; this was greater for nurses working in the outpatient or day surgery departments than in the inpatient settings (Blöndal et al., 2014).
A study at a Brazilian university hospital also found that nurses had supportive attitudes regarding family participation in nursing care; however, attitudes of lower support were noted for nurses who were older, had spent more time in the profession, and had no previous education on family nursing (Angelo et al., 2014). Positive perceptions of family nursing practice were correlated with Taiwanese mental health nurses who had more years of experience in mental health, greater empathy, more supportive attitudes toward the importance of family nursing care, and more personal experiences with family members with serious illness (Hsiao & Tsai, 2015).
Findings from studies surveying nurses with the FINC-NA can be used to guide nurse education on principles of family nursing. No studies have been found by the current authors using the FINC-NA with nurses in the United States. The purpose of this study was to characterize inpatient oncology nurses’ attitudes toward families’ importance in nursing care. A secondary purpose was to determine characteristics of oncology nurses in relation to these attitudes.
Methods
A descriptive, cross-sectional design was used for this observational study. A single set of measurements from inpatient oncology nurses was obtained. The study received approval from the Nursing Research and Innovation Council at the H. Lee Moffitt Cancer Center and Research Institute in Tampa, Florida. In addition, approval was obtained from the cancer center’s scientific review committee and the Advarra Institutional Review Board in Columbia, Maryland.
Sample and Setting
The study was conducted at a National Cancer Institute–designated comprehensive cancer center with Magnet® designation based in the southeastern United States. The survey was distributed to all eligible inpatient oncology nurses (N = 401). Nurses were eligible if they worked in the inpatient setting in a direct care role and had the ability to read and write English. Nurses were excluded if they worked in a non–direct care role, such as management or support (e.g., wound care nurse, ostomy care nurse, continence nurse, case manager, clinical nurse specialist), or were participating in new hire orientation. Data were collected from March to July 2019.
Study Variables
The main outcome variable of interest was nurses’ attitudes toward families’ importance in nursing care, as measured by the FINC-NA. Attitudes are important when acknowledging the family experience of health and illness (Benzein, Johansson, Årestedt, Berg, & Saveman, 2008). The creators of the FINC-NA recognized the need to measure a nurse’s ability to not only recognize families as vital care providers to their ill family member but also as vital members of the care team (Benzein, Johansson, Årestedt, Berg, & Saveman, 2008).
Data Collection
Data were collected by the study team members who rounded on units and attended staff meetings to promote the study and answer questions. A waiver for informed consent was received because this study did not involve patients. Interested nurses completed the demographic data form and the FINC-NA. Once all data were collected, statistical analysis was performed.
Demographic data form: The following demographic information was collected: age range, gender, highest nursing degree, national certifications, marital status, race, ethnicity, religion, length of time as a nurse, length of time at current cancer center, employment status, position, employment type, general approach to the care of families, unit description, and whether a family member had been seriously ill and in need of professional care.
FINC-NA: The outcome variable of attitudes toward families’ importance in nursing care was measured by the FINC-NA. The FINC-NA consists of 26 general statements about the importance of the family in nursing care. Responses are rated on a five-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores are indicative of a more supportive attitude toward families. Nurses are asked to respond to the statements quickly, giving the first reaction that comes to mind. There is a section for comments at the end. Family is defined as the patient/client and family members, friends, neighbors, or significant others (Saveman et al., 2011). The FINC-NA consists of four subscales: family as a resource in nursing care, family as a conversational partner, family as a burden, and family as its own resource. Test-retest reliability was satisfactory for all scales, and intraclass correlation was strongest for the FINC-NA total scale (0.89). None of the scales showed alpha values below 0.7 for internal consistency (Saveman et al., 2011).
Data Analysis
Nurse characteristics were categorized and summarized using frequencies and percentages. Time variables (time as nurse and time at current cancer center) were summarized using median and interquartile range (IQR). To address the first study objective, examination of inpatient nurses’ attitudes toward families’ importance in nursing care, FINC-NA items were described using means, standard deviations, medians, and IQR. For the second study objective, analysis of variance and Pearson correlation were used to assess the relationship between nurse characteristics and attitudes of families’ importance.
Results
Sample Characteristics
A total of 239 nurses completed the survey (60% response rate). Participants tended to be female, aged younger than 40 years, educated with a bachelor’s degree, and employed full-time. The nurses were predominately White and non-Hispanic, and most listed Christian for their religious affiliation (see Table 1). 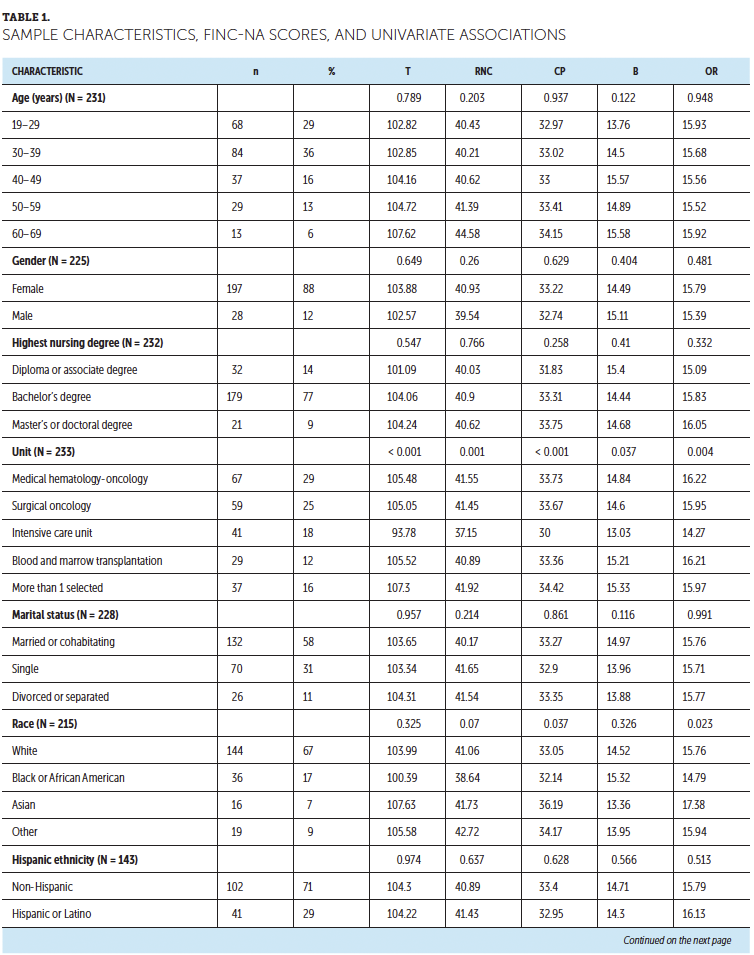
Objective 1: Characterizing Inpatient Nurses’ Attitudes Toward Families’ Importance in Nursing Care
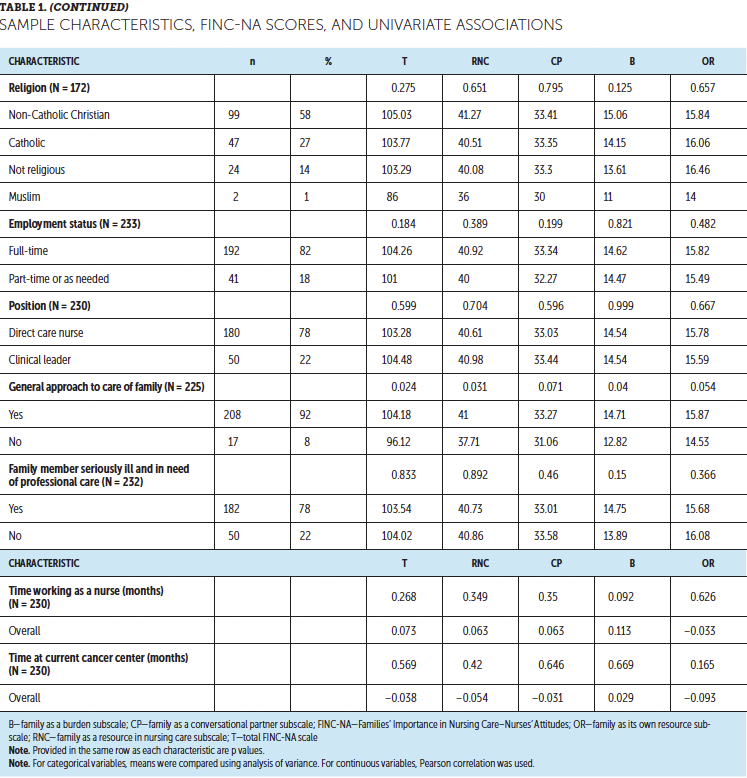
Overall, all item means were above the midpoint on the 1–5 response scale (range = 3.21 [“the presence of family members eases my workload”] to 4.51 [“family members should be invited to actively take part in the patient’s nursing care”]). Table 2 provides the rank-ordered item means and standard deviations (SDs). The median and mean total scores for the FINC-NA were 106 (IQR = 95–113) and 103.61 (SD = 14.1), respectively, of a possible 130. The median and mean subscale scores, respectively, were as follows: family as a resource in nursing care = 41 (IQR = 37–45.5) and 40.69 (SD = 6.05) of a possible 50; family as a conversational partner = 33 (IQR = 30–37) and 33.11 (SD = 4.83) of a possible 40; family as a burden = 15 (IQR = 12–18) and 14.62 (SD = 3.65) of a possible 20; and family as its own resource = 16 (IQR = 14–18) and 15.76 (SD = 2.73) of a possible 20. 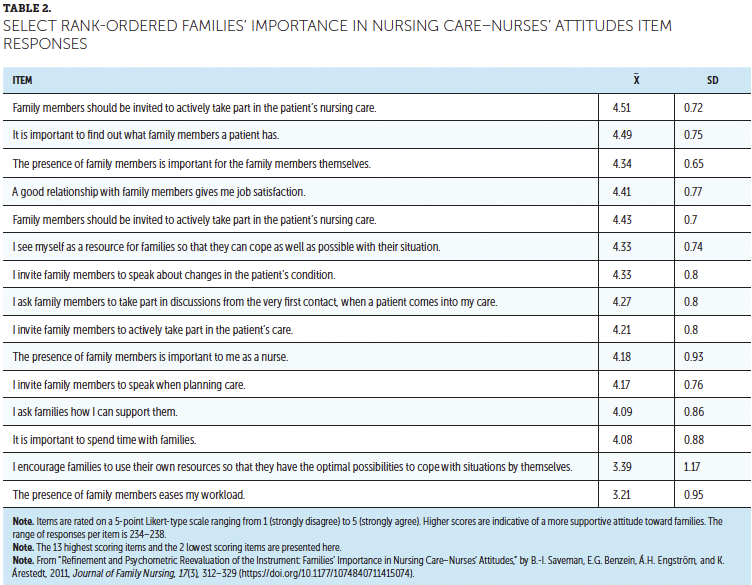
Objective 2: Characteristics of Nurses Related to These Attitudes
Overall FINC-NA scores were related to hospital unit; the intensive care unit had a lower mean (93.78) than the other units. All FINC-NA subscales also were related to hospital unit with the same pattern (intensive care unit less than other units; for all, p < 0.04). Overall scores also were related to having a general approach to the care of family (yes greater than no; p = 0.02). General approach to care also was related to the family as a resource in nursing care subscale (p = 0.03) and the family as a burden subscale (p = 0.04). No other nurse characteristic was related to overall FINC-NA scores.
Discussion
This study examined inpatient oncology nurses’ attitudes toward families’ importance in nursing care. Nurses scored above the midpoint for all the items on the FINC-NA, suggesting that the nurses have a supportive attitude and place high importance on families and their involvement in nursing care activities. Two of the top three highest scoring items were from the family as a resource in nursing care subscale: “family members should be invited to actively take part in the patient’s nursing care” (highest) and “the presence of family members is important for the family members themselves” (third highest). The second highest scoring item, “it is important to find out what family members a patient has,” reflects the family as a conversational partner subscale. These findings are consistent with those from Blöndal et al. (2014) and Luttick et al. (2017). Valuing family presence and including family in conversations surrounding nursing care (Benzein, Johansson, Årestedt, & Saveman, 2008) are aspects of a patient- and family-centered care approach (Nickel et al., 2018).
Although all items scored above the midpoint, the lower scoring items can present as opportunities for focused improvement. The two lowest scoring items, “the presence of family members eases my workload” and “I encourage families to use their own resources so that they have the optimal possibilities to cope with situations by themselves,” represent the family as a resource in nursing care and family as its own resource subscales, respectively. These items may reflect a demanding workload and, as a result, difficulty with building a cooperative and collaborative partnership (Benzein, Johansson, Årestedt, & Saveman, 2008).
Nurse characteristics related to these attitudes were also examined. The characteristics of hospital unit and having a general approach to care were found to be significantly related to attitudes, either for the total scale or subscales. Hospital unit was significant for all scales and suggests that nurses working in the intensive care environment have a less supportive attitude related to the importance of family in nursing care, which may reflect the workload and environment. These characteristics were not found in other studies (Angelo et al., 2014; Benzein, Johansson, Årestedt, & Saveman, 2008; Blöndal et al., 2014; Gusdal et al., 2017; Hsiao & Tsai, 2015; Luttik et al., 2017). Having a general approach to care of the family was identified as significantly affecting attitudes for the total scale; this was similar to findings in other studies (Benzein, Johansson, Årestedt, & Saveman, 2008; Gusdal et al., 2017). Having a general approach was also significantly associated with the family as a resource in nursing care and the family as a burden (negatively scored) subscales, suggesting that the hallmarks of a patient- and family-centered approach support the importance of valuing the presence of family, having good nurse–family relationships, and taking time to care for families (Benzein, Johansson, Årestedt, & Saveman, 2008; Nickel et al., 2018).
Attitudes are formed through psychological processes by comparing the negative and positive attributes of an object, person, or group to past experiences (Alves et al., 2020; Bakanauskas et al., 2020). Starting in childhood, parents and other close environmental influences express their attitudes and views on the dichotomous nature of what is good or bad, right or wrong, and positive or negative (Bakanauskas et al., 2020). In turn, these attitudes guide behavior and decisions on whether one likes or dislikes or behaves favorably or unfavorably toward an object, person, or group (Alves et al., 2020; Bakanauskas et al., 2020; Price, 2015). Attitude formation continues throughout life. Social groups and organizations continue to influence attitudes and subsequent behaviors (Bakanauskas et al., 2020). Nurses learn the desired attitudes of nursing through socialization into the profession, often through training and reflection (Price, 2015). Understanding the behaviors of themselves and others helps nurses deliver quality patient- and family-centered care (Price, 2015).
To enculturate new nurses to the cancer center’s primary focus of providing quality care to patients and their families, orientation includes lectures on the cancer center’s nursing vision, values, and philosophy; personalized patient- and family-centered care; and principles of Duffy’s (2018) quality caring model. This model emphasizes caring factors such as acknowledging feelings, fears, and hopes; taking the time to meet emotional and physical needs; addressing patients’ and family members’ questions; providing interprofessional education; and mutually deciding on a plan of care. New hires are also required to participate in the center’s Promise training (Moffitt Cancer Center, 2017), which integrates the four core concepts of patient- and family-centered care: dignity and respect, information sharing, participation, and collaboration. The Promise is intended to provide compassionate, connected, and exceptional care to patients, caregivers, and one another every day in every way, and it includes measurable standards of behavior and language.
Patient- and family-centered care extends beyond orientation. Nurses continue to engage the patient and their family with the Promise to put the patient first, demonstrate attentive respect, and share information in a compassionate, courteous manner. Promise 2.0 training is facilitated by the cancer center’s patient experience and staff nurse advisory council; it consists of an introductory web-based training titled Promise on the Job: A Review Course and three 30-minute virtual sessions centered around a discussion of case scenarios occurring during a six-month period. Staff also are trained to use the AIDET® framework (Barber, 2018), which stands for acknowledge, introduce, duration, explanation, and thank you, when communicating with patients and family members. Having awareness of and acknowledging patients’ experiences, including patients in their care, and seeing the whole patient and their family continue to be emphasized. Consistent training and protocols can guide nurses in the assessment of this clinical care area and the development of interventions.
Limitations
This study was limited to inpatient oncology nurses at one cancer center in the southeastern United States. In addition, the primary instrument used was not designed for specific settings. Consequently, these results are not generalizable to other specialties, geographic locations, cultures, or outpatient settings. There was limited representation based on gender. Other factors that may influence attitudes toward family importance, such as regional religious and secular cultures, were not included. These results represent a single administration of the survey with a response rate of 60%.
Implications for Nursing
Findings from this study can be used for training clinical oncology nurses in practice. A potential contribution of this study is that it provides a measurement of inpatient oncology nurses’ attitudes toward family involvement in care. This information can be used in the development of educational strategies and support programs for nursing staff regarding families’ importance and involvement in patients’ care. Hospitalized patients with cancer tend to be much sicker than ambulatory care patients and are often at the end of life, a factor that could greatly affect nurses’ attitudes toward families. Because most care of patients with cancer occurs in ambulatory settings, evaluating the ambulatory care oncology nurse’s attitude of families’ importance in care should be considered.
Implications for Research
Future research may include examining the relationship between family support and patient outcomes, with the goal of advancing nursing practice and improving the patient and family experience. The integration of the FINC-NA adds to the reliability of the instrument with inpatient oncology nurses. This study design is associated with a one-time view of nurses’ attitudes and presents an initial approach in the study of this area. Additional studies are warranted, including a longitudinal approach and qualitative methods. A uniform assessment and/or the use of tools to assess nurses’ attitudes would be beneficial; this could include an instrument for use in the ambulatory setting. Because care is premised on engagement of the family and on the relationships between family caregivers and the nurse, future research should also consider diversity, such as race, ethnicity, and religion. Consideration of employment setting, geographic region, and nursing specialty, as well as inpatient versus outpatient care, is also warranted to understand attitudes toward families’ importance in care and to implement strategies that optimize patient and family experiences. 
Conclusion
Patient- and family-centered models of care place a strong emphasis on acknowledging the family’s experience of health and illness; care occurs in collaboration with the active participation of patients and families as members of the healthcare team. Attitudes of nurses have been found to have a relationship with family support and patient outcomes; as a result, there is a need to examine these attitudes. Exploring these attitudes with an instrument such as the FINC-NA can guide the creation of effective initiatives for improving the patient experience. 
About the Author(s)
Tina M. Mason, PhD, APRN, AOCN®, AOCNS®, FCNS, is a nurse researcher, Richard R. Reich, PhD, is the manager of the Biostatistics and Bioinformatics Shared Resource, Rhonda Musgrove, BSN, RN, WOC, is an RN and a wound, ostomy, and continence nurse, Junmin Whiting, PhD, is a biostatistician II, and Jane Fusilero, RN, MSN, MBA, is the vice president of care services and chief nursing officer, all at the H. Lee Moffit Cancer Center and Research Institute in Tampa, FL. The authors take full responsibility for this content. This work was supported, in part, by the Biostatistics and Bioinformatics Shared Resource at the H. Lee Moffitt Cancer Center and Research Institute, a National Cancer Institute–designated comprehensive cancer center (P30-CA076292). The article has been reviewed by independent reviewers to ensure that it is objective and free from bias. Mason can be reached at tina.mason@moffitt.org, with copy to CJONEditor@ons.org. (Submitted December 2020. Accepted March 9, 2021.)
References
Alshahrani, S., Magarey, J., & Kitson, A. (2018). Relatives’ involvement in the care of patients in acute medical wards in two different countries—An ethnographic study. Journal of Clinical Nursing, 27(11–12), 2333–2345. https://doi.org/10.1111/jocn.14337
Alves, H., Högden, F., Gast, A., Aust, F., & Unkelbach, C. (2020). Attitudes from mere co-occurrences are guided by differentiation. Journal of Personality and Social Psychology, 119(3), 560–581. https://doi.org/10.1037/pspa0000193
Angelo, M., Cruz, A.C., Mekitarian, F.F.P., da Silva dos Santos, C.C., Costa Marques Martinho, M.J., & da Silva Martins, M.M.F.P. (2014). Nurses’ attitudes regarding the importance of families in pediatric nursing care. Revista da Escola de Enfermagem da USP, 48, 74–79.
Bakanauskas, A.P., Kondrotienė, E., & Puksas, A. (2020). The theoretical aspects of attitude formation factors and their impact on health behaviour. Management of Organizations: Systematic Research, 83(1), 15–36. https://doi.org/10.1515/mosr-2020-0002
Barber, S. (2018). Patient care in decline: AIDET as a tool for improvement. Radiologic Technology, 89(4), 419–421.
Benzein, E., Johansson, P., Årestedt, K.F., Berg, A., & Saveman, B.-I. (2008). Families’ importance in nursing care: Nurses’ attitudes—An instrument development. Journal of Family Nursing, 14(1), 97–117. https://doi.org/10.1177/1074840707312716
Benzein, E., Johansson, P., Årestedt, K.F., & Saveman, B.-I. (2008). Nurses’ attitudes about the importance of families in nursing care: A survey of Swedish nurses. Journal of Family Nursing, 14(2), 162–180. https://doi.org/10.1177/1074840708317058
Blöndal, K., Zoëga, S., Hafsteinsdottir, J.E., Olafsdottir, O.A., Thorvardardottir, A.B., Hafsteinsdottir, S.A., & Sveinsdøttir, H. (2014). Attitudes of registered and licensed practical nurses about the importance of families in surgical hospital units: Findings from the Landspitali University Hospital Family Nursing Implementation Project. Journal of Family Nursing, 20(3), 355–375.
Dahlke, S., Steil, K., Freund-Heritage, R., Colborne, M., Labonte, S., & Wagg, A. (2018). Older people and their families’ perceptions about their experiences with interprofessional teams. Nursing Open, 5(2), 158–166. https://doi.org/10.1002/nop2.123
Duffy, J.R. (2018). Quality caring in nursing and health systems: Implications for clinicians, educators, and leaders (3rd ed.). Springer.
Gusdal, A.K., Josefsson, K., Thors Adolfsson, E., & Martin, L. (2017). Nurses’ attitudes toward family importance in heart failure care. European Journal of Cardiovascular Nursing, 16(3), 256–266. https://doi.org/10.1177/1474515116687178
Hetland, B., Hickman, R., McAndrew, N., & Daly, B. (2017). Factors influencing active family engagement in care among critical care nurses. AACN Advanced Critical Care, 28(2), 160–170. https://doi.org/10.4037/aacnacc2017118
Hsiao, C.-Y., & Tsai, Y.-F. (2015). Factors associated with the perception of family nursing practice among mental health nurses in Taiwan. Journal of Family Nursing, 21(4), 508–528.
Institute for Patient- and Family-Centered Care. (n.d.). Patient- and family-centered care. https://www.ipfcc.org/about/pfcc.html
Koren, D., Laidsaar-Powell, R., Tilden, W., Latt, M., & Butow, P. (2018). Health care providers’ perceptions of family caregivers’ involvement in consultations within a geriatric hospital setting. Geriatric Nursing, 39(4), 419–427. https://doi.org/10.1016/j.gerinurse.2017.12.013
Luttik, M.L.A., Goossens, E., Ågren, S., Jaarsma, T., Mårtensson, J., Thompson, D.R., . . . Strömberg, A. (2017). Attitudes of nurses towards family involvement in the care for patients with cardiovascular diseases. European Journal of Cardiovascular Nursing, 16(4), 299–308.
Moffitt Cancer Center. (2017). The Moffitt Promise. https://bit.ly/3sDaQyZ
Nickel, W.K., Weinberger, S.E., & Guze, P.A. (2018). Principles for patient and family partnership in care: An American College of Physicians position paper. Annals of Internal Medicine, 169(11), 796–799. https://doi.org/10.7326/M18-0018
Nyborg, I., Danbolt, L.J., & Kirkevold, M. (2017). User participation is a family matter: A multiple case study of the experiences of older, hospitalised people and their relatives. Journal of Clinical Nursing, 26(23–24), 4353–4363. https://doi.org/10.1111/jocn.13765
Price, B. (2015). Understanding attitudes and their effects on nursing practice. Nursing Standard, 30(15), 50–60. https://doi.org/10.7748/ns.30.15.50.s51
Saveman, B.-I., Benzein, E.G., Engström, Å.H., & Årestedt, K. (2011). Refinement and psychometric reevaluation of the instrument: Families’ Importance in Nursing Care—Nurses’ Attitudes. Journal of Family Nursing, 17(3), 312–329.
Sivertsen, D.M., Lawson-Smith, L., & Lindhardt, T. (2018). What relatives of older medical patients want us to know—A mixed-methods study. BMC Nursing, 17, 32.
Sofaer, S., & Schumann, M.J. (2013). Nursing Alliance for Quality Care white paper on patient engagement. https://bit.ly/3gshDGW

